Definition
Prolonged penile erection (>4 hours), continues without sexual stimulation and despite ejaculation/orgasm.
Classification
Ischaemic (low flow) – more common. Painful due to ischaemia, with pain increasing with the duration of the priapism. Caused by venous outflow obstruction/thrombosis. Presents as rigid erection sparing the glans. If persists >12 hours, priapism can lead to permanent fibrosis and calcification. Causes: idiopathic, haematological (eg sickle cell disease) and medication (vasoactive erectile agents, antipsychotics, anticoagulants, antidepressants, anti-hypertensives, hormone therapy).
Non-ischaemic (high flow) – less common. Painless or only uncomfortable with no risk of necrosis. Normally secondary to trauma, unregulated inflow due to rupture of cavernosal artery.
Rarer subtypes:
- Recurrent/stuttering – more common in sickle cell disease patients. Frequent prolonged and painful erections. Treatment involves oxygenation, hydration, analgesia and possible exchange transfusion.
- Priapism in spinal shock – occurs in spinal injury with loss of sympathetic tone leading to high-flow, non-ischaemic priapism. Requires no treatment.
If in doubt, manage as ischaemic priapism
Clinical History
If possible, establish and document
- Duration of erection (<48 hours, 48-72 hours, >72 hours)
- Any underlying haematological disorder
- Current medication
- Illicit drug use
- Symptoms to suggest pelvic malignancy
- Previous episodes
- Recent perineal/penile trauma
- Neurological symptoms
Examination
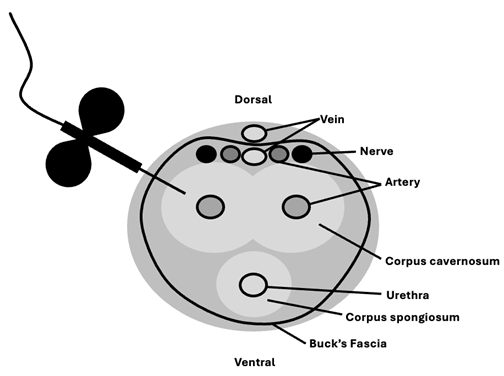
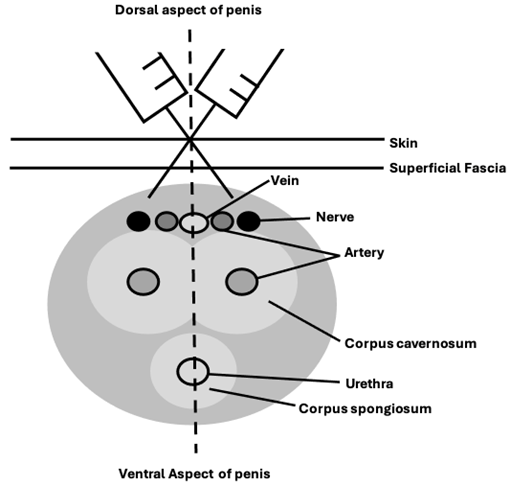
- Penis – look for evidence of sparing of the glans and trauma
- Abdomen and DRE – look for evidence of underlying pelvic malignancy
- Neurological – evidence of spinal cord injury
Investigations (if available)
- Bloods – FBC, electrolytes, clotting, blood smear/sickle cell screen
- Urine and blood toxicology if recreational drug use
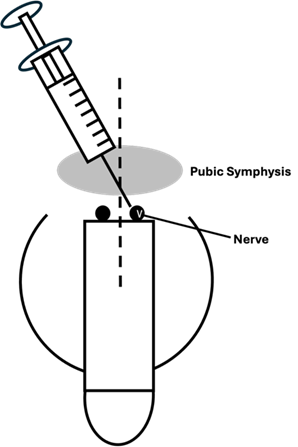
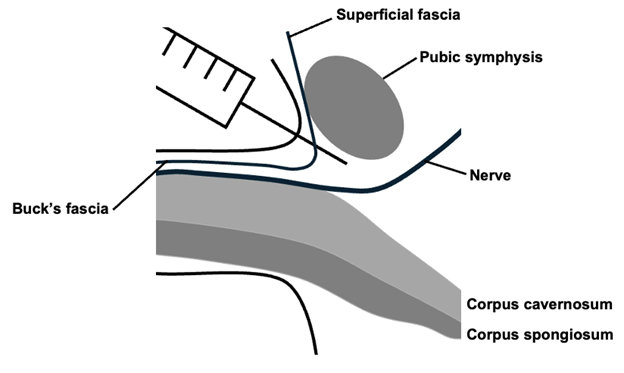
- Penile bloods gas from first aspirate to help differentiate ischaemic (pH <7.25, pCO2 >8 kPa, pO2 <4 kPa) and non-ischaemic priapism but normoxia does not exclude ischemic priapism.
- Imaging
- US penile doppler
- Abdominal and pelvic CT/MRI – penile MRI can be used to assess viability of corpus cavernosum in refractory cases
Management
Ischaemic – for patients with prolonged priapism or priapism that proves refractory to the above interventions, Urology specialist input is required for surgical shunt formation and consideration of early penile prosthesis insertion
Non-ischaemic – manage conservatively. If does not spontaneously resolve, will need specialist intervention in a unit that can offer super selective arteriography and embolization.
Follow up
All patients will need specialist follow-up to monitor for late-onset erectile dysfunction