Embedded unexploded ordnance (UXO)
Objectives
To describe the principles and management of embedded unexploded ordnance during surgical management of injured personnel
Scope
The guideline covers the considerations during the safe removal of UXO, and how to manage patients who require surgery with embedded UXO.
Audience
Relevant to all healthcare providers during the management of injured patients, including Emergency Medicine physicians, General & Vascular surgeons, Trauma & Orthopaedic surgeons, Anaesthetic and ICU teams, Perioperative Practitioners and nursing staff.
Initial Assessment & Management
Initial inspection
- All patients, regardless of whether they are friendly or enemy, require an initial inspection to find and remove all weapons and ammunition prior to entry into a transport vehicle or MTF and before medical evacuation.
- Screening of all carried materials is essential to ensure that no loose ordnance is brought into an area where they could be accidentally armed and detonated.
- Items must be conveyed to the unit representatives or the area Explosive Ordnance Disposal (EOD) team, or placed in a safe location (e.g. UXO pit) if the former options are not safe to do so.
Immediate actions on discovery of UXO
- All nonessential individuals should transfer to a safe location and the chain of command be notified.
- The principles of the 4Cs (Confirm, Clear, Cordon, Control) provide a useful structure to follow.
- Once the UXO is removed, it should be gently transferred to a designated secure area. If the UXO is placed in a containment device in the vicinity of the patient, consider rapidly moving the patient to a safer location to complete the surgery or ask EOD for advice.
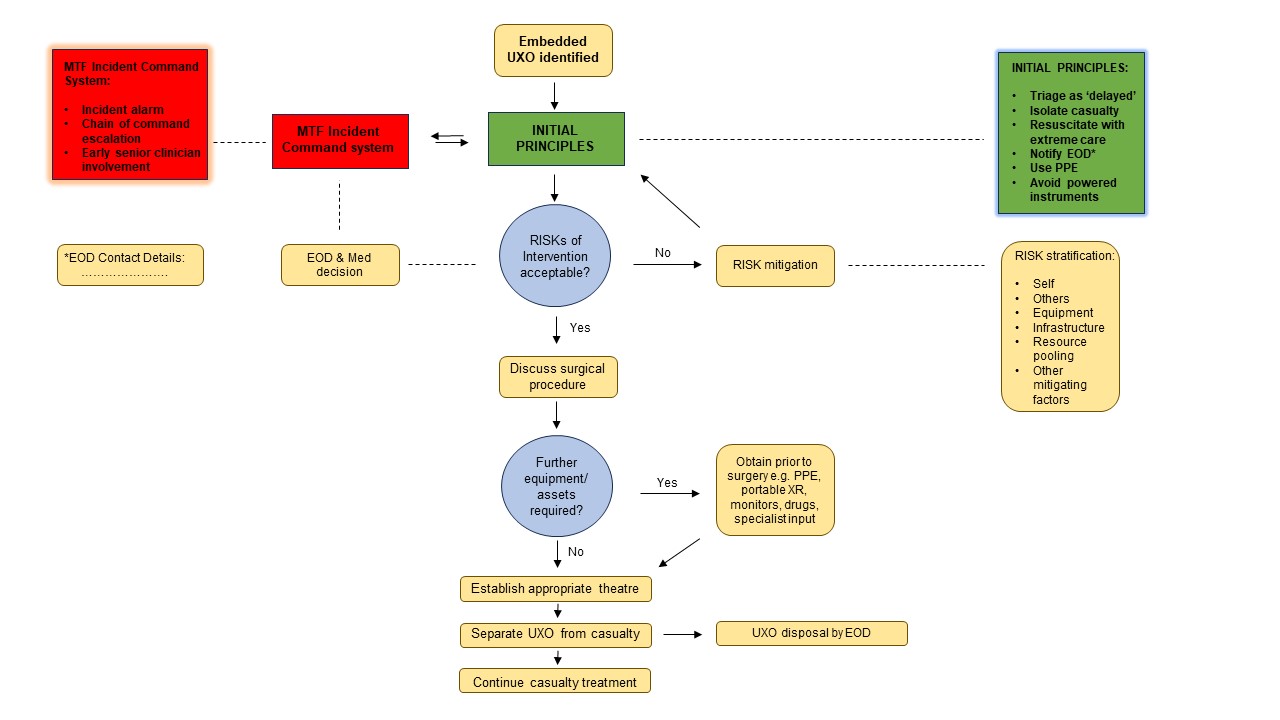
Risk Management and Informed decision making
- The balance of risk from an embedded UXO must be assessed at every stage of the care pathway with the potential benefit to the casualty weighed against the potential risk to personnel and infrastructure.
- Once the alarm has been raised regarding an embedded UXO in a casualty arriving at an MTF, early senior clinician and EOD involvement will be required, with regular liaison with the chain of command.
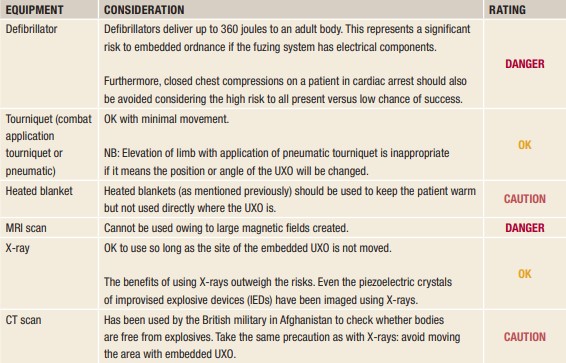
- Once the decision to treat a casualty with embedded UXO has been taken, serious consideration must be given to what specific equipment could be used and how it should be used. Some UXO items are more sensitive than others; in the case of manufactured military ordnance, it is generally the fusing system which dictates the sensitivity.
ICRC publication, ‘Removing Embedded Ordnance From Patients’
Factors to consider during medical treatment of patients with embedded UXO to avoid inadvertent detonation (from ICRC)
|
Factor |
Consideration |
Guidance |
|
Movement
|
Some fuses can be activated with the slightest knock (e.g primed striker, piezoelectric crystals). |
Keep ordnance in same orientation Limb elevation may not be possible. Optimise analgesia to settle agitation; RSI may be required |
|
Vibration and friction
|
Internal components of UXO can be exposed after initial impact, which can include highly sensitive explosive compositions. |
Ensure potential sources of friction are removed, especially during patient transport. Limit mechanical equipment during treatment. |
|
Temperature changes
|
It is important to keep patient warm. Different blankets can exert properties that may impact upon the UXO e.g exothermic reactions (heated blanket), static build-up (reflective space blanket) |
Always take a balanced approach: the shivering of a hypothermic patient may pose a bigger risk of detonation than the warmth of a heated blanket |
|
Radio-frequency energy
|
Very high and ultrahigh frequency (VHF and UHF) radio transmissions are particularly dangerous when there are exposed detonator leads. |
VHF transmissions and mobile phone calls should be made at least 15 metres away from the patient. |
|
Static electricity, electric current and strong magnetic fields
|
Certain fuses use electric current, particularly in impact or proximity sensing. Static electricity is an ignition hazard. Strong magnetic fields can also affect piezoelectric crystals |
Everyone who treats or otherwise touches the patient must earth/ground themselves first. Avoid strong magnetic fields near RPGs. |
Management pathway after the discovery of UXO in an injured patient
Advanced Assessment & Management
Principles during surgery
- The overall principle is to remove the UXO by the most expedient means possible. This may require en-bloc resection of the tissue around the ordnance with amputation of the affected limb above the ordnance if this is deemed the quickest way to safely remove the ordnance.
- In general, embedded ordnance should be surgically exposed to a degree that will allow easy removal of the object in the same orientation as it lies in the body.
- Every effort should be attempted to avoid pushing forward or twisting the UXO during exposure or removal as this may set off a triggering mechanism.
- Great care should be made to avoid knocking or contacting the ordnance with hands or surgical instruments.
- If ordnance is embedded into a limb, the extremity should be stabilised to avoid excessive vibration or movement that could complete the triggering mechanism leading to detonation.
- Surgery for other injuries should be limited to those essential to preserve life, and all definitive procedures should be delayed until after the ordnance is safely removed.
- Use of electrocautery, mechanical blood warmers, monitors, blood pressure gauges, infusers, or pumps should be minimised in order to reduce the risk of static electrical discharge
- Furthermore, mechanical saws and drills that use electricity, and any pneumatic instruments should also be avoided due to concerns of discharge and vibrations.
- Combustible agents in vicinity of the patient should be limited as far as possible according to a risk benefit analysis (e.g., oxygen, alcohol-based solution, combustible volatile anaesthetics).
Personnel deemed not essential to achieve safe removal should move away at least 100m from the vicinity of the UXO. A surgical assistant should only be used if it is essential and the safe removal of the UXO could not otherwise be accomplished.
Anaesthetic considerations
General anaesthetic will be used for these operations since it provides a more controlled environment. For stable patients where the UXO is embedded in an extremity, a nerve block may be an acceptable alternative. Supplemental oxygen during the operation should be used judiciously in order to reduce the risk of combustion, although this should be lower risk if a contained ventilation circuit is used.
Prolonged Casualty Care
Not applicable
Paediatric Considerations
No different to adult
